Osteoporosis
Guide I-105
Revised by Sonja Koukel and Desaree Jimenez
College of Agricultural, Consumer and Environmental Sciences, New Mexico State University
Authors: Respectively, Assistant Professor/Extension Community and Environmental Health Specialist, Department of Family and Consumer Sciences; and Extension Home Economist, Rio Arriba County Extension Office, New Mexico State University. (Print friendly PDF)
Introduction
Osteoporosis is a major health problem in the United States, afflicting an estimated 10 million adults. About 34 million adults have low bone mass, or osteopenia, a condition that places them at high risk for osteoporosis. While these numbers are staggering, many individuals go undiagnosed. About 30% of postmenopausal women have osteoporosis, but only about 2% are diagnosed and treated. And although osteoporosis is considered a woman's disease, more than 30% of all men will be affected by the age of 75.
What Is Osteoporosis?
Osteoporosis is a condition of bone softening or deterioration or loss of bone mineral density that leads to disability, bone fractures, and even death from medical complications. The disease occurs when the bones become porous through a loss of minerals, particularly calcium (Figure 1). A decrease in bone mass can result in bones that are weak, fragile, and brittle. In this condition, bones—particularly the hips, wrists, ribs, and spine—are more prone to fractures and breaking.
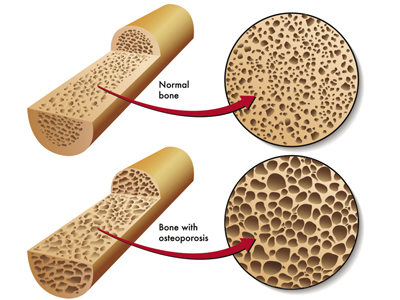
Figure 1. A comparison of healthy bones (top) and bones with mineral loss due to osteoporosis (bottom). © Rob3000/Dreamstime.com. Used with permission.
What Are the Symptoms of Osteoporosis?
Osteoporosis has been termed a "silent" disease because of the lack of any symptoms. Fractures are the biggest consequence of osteoporosis. People may not know they have osteoporosis until their bones become so weak that a sudden strain, bump, or fall causes a bone to fracture.
What Are the Effects of Osteoporosis?
Bone fractures and breaks resulting from osteoporosis may not be the worst health challenges for older adults. The disease may also cause pain, lower quality of life, and crippling. Older adults who are bedridden as a result of a fracture or break experience weakness and are more vulnerable to infections. Sadly, health statistics report that up to 20% of older adults who suffer a hip fracture die within a year due to complications.
Who Is at Risk for Osteoporosis?
Although osteoporosis can strike at any age, it mostly affects adults aged 50 and older. While both men and women can develop osteoporosis, women are four times more likely than men to develop the disease. Compared with men, women have less bone mass to begin with and lose it at a faster rate. Loss of bone mass occurs especially in the years just before menopause and for the first five years following the end of menstrual periods. This situation is partly due to the loss of estrogen, a natural hormone that helps deposit calcium in bones.
Caucasian (non-Hispanic white) and Asian women are at the highest risk of developing osteoporosis, Latinos and Native Americans are at moderate risk, and African American women and men are the lowest risk. However, it is important to remember that everyone loses bone mass as they age, regardless of gender or ethnicity, so it's important to take control of your health and keep the disease at bay. Other risk factors that contribute to osteoporosis are:
• Age over 50
• Current low bone mass
• White or Asian ethnicity
• Heavy consumption of alcohol
• Inactive lifestyle and immobility (e.g., bed or wheelchair confinement)
• Lack of physical activity or exercise
• Deficiency in vitamin D
• Having a diet low in calcium throughout your life
• Overuse of certain medications, such as corticosteroids (man-made steroids)
• Eating disorders (e.g., anorexia nervosa)
• Smoking
• Family history of osteoporosis
• Thin or small body frame
• Female
• History of abnormal absence of menstrual periods
• Early menopause — before age 45
• Women: Estrogen deficiency resulting from early menopause (before age 45), menopause, or surgical removal of the ovaries
• Men: Low testosterone levels
How Can Osteoporosis Be Prevented?
Osteoporosis can be prevented through a combination of proper diet and regular exercise. The National Institutes of Health recommend getting the daily recommended amounts of calcium and vitamin D in your diet. Weight-bearing or load-bearing exercises can help preserve bone density.
Calcium
Calcium is a mineral that is necessary for life. In addition to building bones and keeping them healthy, calcium helps the blood to clot, the nerves to send messages, and the muscles to contract, along with other bodily functions. Adequate calcium intake is also associated with a reduced risk for colon cancer in men and women.
About 99% of the calcium in our bodies is located in the bones and teeth. Each day, you lose calcium through your skin, nails, hair, sweat, urine, and feces. Because our bodies cannot produce calcium, it's important to get enough calcium through the foods we eat. When you don't get enough calcium, your body takes the calcium it needs from your bones.
The recommended dietary allowance (RDA) for calcium is between 1,000 and 1,300 milligrams (mg) per day. Experts in this area recommend higher intakes. Table 1 lists the recommended daily calcium intake for different age groups.
The best way to get the daily calcium requirement is through calcium-rich foods, including calcium-fortified foods. Table 2 provides a short list of low-fat, calcium-rich foods.
Table 1. Recommended Daily Calcium Intake
|
Age |
Amount (mg)
|
| 1—5 |
800
|
| 6—10 |
800—1,200
|
| 11—24 |
1,200—1,500
|
| 25—50 Women |
1,000
|
| 25—64 Men |
1,000
|
| Post-menopausal women who ARE on HRT* |
1,000
|
| Post-menopausal women who ARE NOT on HRT* |
1,500
|
| Adults over 65 years of age |
1,200—1,500
|
| *HRT — Hormone replacement therapy | |
Table 2. Low-Fat, Calcium-Rich Foods
|
Calcium (mg) |
Food
|
Serving
|
|
448
|
Yogurt, low-fat, plain |
1 cup
|
|
368
|
Soy milk, calcium-fortified |
1 cup
|
|
300
|
Orange juice, calcium-fortified |
1 cup
|
|
296
|
Milk, skim |
1 cup
|
|
180
|
Salmon, canned with bones |
3 ounces
|
|
158
|
Bok choy (Chinese cabbage)* |
1 cup
|
|
125
|
Beans, white navy* |
1 cup
|
|
109
|
Oatmeal, instant, calclium-fortified, plain |
1/2 cup
|
|
100
|
Almonds, dry roasted |
1/4 cup
|
|
94
|
Kale* |
1 cup
|
|
78
|
Cottage cheese, 2% low-fat |
1/2 cup
|
|
72
|
Broccoli* |
1 cup
|
|
56
|
Spinach* |
1 cup
|
| *Calcium content remains the same whether raw or cooked. | ||
Calcium Supplements
Food should be your first choice for calcium sources. However, most people don't get enough calcium from their daily diet. Calcium supplements can be beneficial for getting adequate levels of calcium. There are two forms of supplements:
• Calcium citrate is well absorbed with or without food.
• Calcium carbonate should be taken with food since food helps with the absorption.
When taking calcium supplements, do not take more than 500 mg at a time; amounts larger than 500 mg are not well absorbed. And don't forget the vitamin D, which is vital for calcium absorption.Vitamin D
Vitamin D plays a major role in protecting bones. Your body needs vitamin D to absorb calcium, making vitamin D the "key" to allowing calcium to be deposited into the bones. Without it, it would be virtually impossible for the body to absorb calcium. Children need vitamin D to build strong bones, and adults need it to keep bones strong and healthy. Low vitamin D levels can cause bone loss, lower bone density, and of course a greater chance for broken bones as we age.
There are three ways to get vitamin D: food, vitamin supplements, and sunlight. About 15 minutes of unprotected sun exposure are required, depending upon skin tone and sun intensity. In the winter months, longer exposure would be needed. If you are not sure you are getting enough vitamin D, visit your healthcare provider and ask for a vitamin D level test.
Good food sources of vitamin D are listed in Table 3. Vitamin D recommendations are measured in international units (IUs), and daily recommendations for different age groups include:
Table 3. Good Food Sources of Vitamin D
|
IU |
Food |
Serving
|
|
360
|
Salmon |
3.5 ounces
|
|
345
|
Mackerel |
3.5 ounces
|
|
250
|
Sardines in oil, drained |
3.5 ounces
|
|
200
|
Shrimp |
3.5 ounces
|
|
100
|
Orange juice, D-fortified |
1 cup
|
|
100
|
Milk, any type, D-fortified |
1 cup
|
|
60
|
Margarine, D-fortified |
1 tablespoon
|
|
60
|
Yogurt, D-fortified |
3/4—1 cup
|
|
40
|
Cereal, D-fortified |
1 cup
|
|
20
|
Egg |
1
|
• 0-12 years of age = 400 IUs
• 1-70 years of age = 600 IUs
• 71 years and older = 800 IUs
Exercise
As stated previously, weight-bearing or load-bearing exercises done on a regular basis have been found to help maintain bone density (Figure 2). While exercises such as swimming and walking are good for the heart and lungs (cardiovascular), they are not very effective at increasing bone health. The best exercises include:

Figure 2. Exercises like weight-lifting can help maintain bone density.
• weight-lifting,
• jogging,
• hiking,
• stair-climbing,
• step aerobics,
• dancing, and
• racquet sports, such as tennis.
Essentially, the most effective activities are those that require your muscles to work against gravity while staying upright. Practice thirty minutes of weight-bearing exercise daily. Those 30 minutes don't need to be done all at once; it's just as effective to do 10 minutes at a time three times daily. Always speak with your healthcare provider about exercising before beginning an exercise program.
What Is a Bone Mineral Density Test?
Your healthcare provider can use a test to measure your bone mass. The bone mineral density (BMD) test is most often done for the spine, wrist, and/or hip. These are the most common fracture sites due to porous bones. The test is painless and non-invasive. It is done using a special type of X-ray. Unlike regular X-rays, this test results in less radiation exposure than you would receive taking an airplane ride from coast to coast. Information can also be obtained from regular X-rays, ultrasound, or a CT (computerized tomography) scan.
Who should get tested? Speak with your healthcare provider about your possible need for a test and where you can get one. The National Osteoporosis Foundation recommends that the following people get tested.• All women age 65 and older.
• Younger postmenopausal women who have one or more risk factors (other than being white, postmenopausal, and female). Refer to the Who Is at Risk for Osteoporosis? section of this publication for risk factors.
• Postmenopausal women who have had a recent fracture.
How Is Osteoporosis Treated?
Osteoporosis is incurable, but steps can be taken to slow or minimize its progression. Nutrition, exercise, medication, and preventing falls are all part of a comprehensive treatment program.
• Nutrition: Healthful eating will always contribute to one's overall health. Getting an appropriate daily intake of calcium and vitamin D is especially important for bone health. Supplements can be an important addition to the daily diet to ensure RDAs are met. (See How Can Osteoporosis Be Prevented? section for dietary suggestions.)
• Exercise: While exercise plays an important role in preventing osteoporosis, it also has an important role in its management. Exercise improves bone strength and enhances muscle coordination and balance (which is important in preventing falls). It can also enhance flexibility. Practice weight-bearing or load-bearing exercises for at least 30 minutes each day.
• Medication: Your doctor can prescribe medication that will help treat osteoporosis.
• Preventing falls: Since osteoporosis weakens bones, they break more easily. Therefore, preventing falls is vitally important. Safety tips include:
-
-
Using a cane or walker as needed.
-
Being careful on, or altogether avoiding, slippery walkways.
-
Wearing shoes that are optimal for traction, such as those with rubber soles. Make sure that shoelaces are securely tied and tucked away.
-
Optimizing your vision; for example, wearing glasses and ensuring proper lighting where you walk.
-
Utilizing handrails for stairways and grab bars in bathrooms, showers, and tubs.
-
Using strong step stools with wide bases and handles.
-
Securing throw rugs in your home. Or, better yet, don't use them at all.
-
Keeping obstacles such as cords and clutter out of walkways in the home.
-
Using a rubber mat in the shower/bathtub.
-
Taking into consideration side effects of medications that may affect balance, mobility, or mental awareness. Talk with your healthcare provider about the possibility of such side effects, and let your doctor know if they occur.
-
Many county Extension offices offer some type of strength-building exercise programs. Contact the Extension office in your county for more information (https://aces.nmsu.edu/county/).
Original authors: Bruce Jacobs, Extension Health Specialist; and M. Ann Bock, Professor, Human Nutrition.

Sonja Koukel is Assistant Professor and Extension Community and Environmental Health Specialist in the Department of Extension Family and Consumer Sciences. She earned her B.S. at NMSU and her M.S. and Ph.D. at Texas Tech University. Her Extension programs focus on health and wellness—physical, mental, spiritual, and environmental.
To find more resources for your business, home, or family, visit the College of Agricultural, Consumer and Environmental Sciences on the World Wide Web at pubs.nmsu.edu
Contents of publications may be freely reproduced for educational purposes. All other rights reserved. For permission to use publications for other purposes, contact pubs@nmsu.edu or the authors listed on the publication.
New Mexico State University is an equal opportunity/affirmative action employer and educator. NMSU and the U.S. Department of Agriculture cooperating.
Revised and electronically published July 2013 Las Cruces, NM